Facts about atopic dermatitis(AD)
- Atopic eczema is a chronic relapsing condition with variability in age of onset and severity.
- Most of the cases (about 80%) have a mild disease.
- The aim of treatment is to control rather than cure.
General instructions
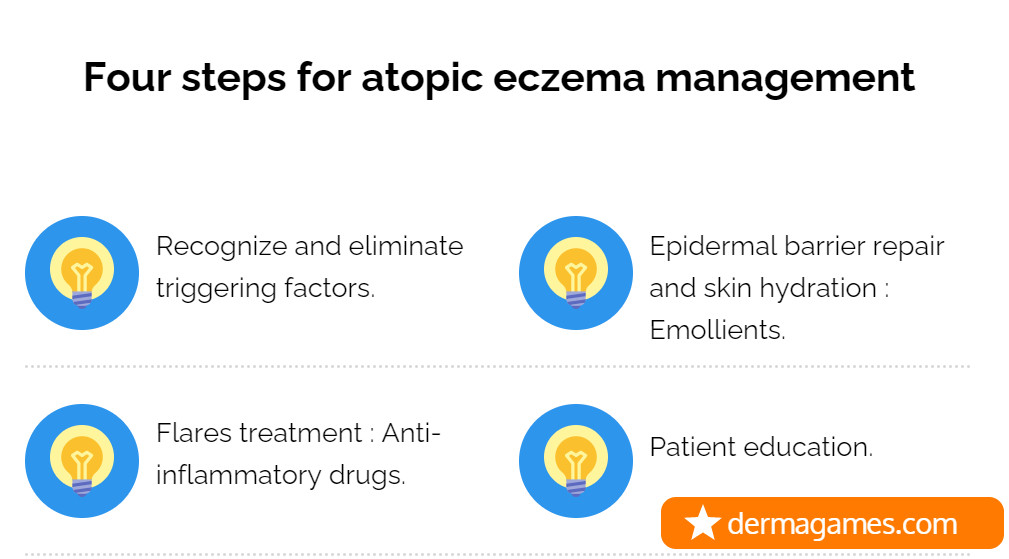
- Complete medical history of the patient`s condition, family history of atopy, home environment and triggering factors surveying should be taken.
- Management plan should be tailored according to the patient needs.
- Treatment options should be based on severity, age of the patient and the affected sites.
- Early treatment of AD is essential as it may prevent other atopic conditions such as allergic rhinitis, asthma and food allergy.
- Emollient therapy and good hydration of the skin are essential.
- Avoid the possible precipitating factors is a crucial step to avoid frequent flares.
- Management plans usually consists of two stages; induction of remission and then maintenance therapy.
- Atopic dermatitis is a stressful condition for both patients and their family.
- Patient education (medical, nutritional, and psychological) is a cornerstone in atopic dermatitis management.

What are the possible triggering factors in atopic patients?
- Irritants (saliva, soaps, detergents, foods, clothing)
- Sweat.
- Drying (central heating).
- Scratching.
- Foods (eggs, cow’s milk, wheat, etc.)
- House dust mites : House dust mites eradication may improve atopic dermatitis.
- Pets.
- Infections.
- Airborne allergens (grass and tree pollens, HDM, animal dander).
- Contact allergies (including topical treatments).
- Stress.
How to assess the severity of atopic eczema ?
- There are multiple scores that have been used to assess the severity eg, the Scoring of Atopic Dermatitis (SCORAD) index, the Eczema Area and Severity Index (EASI), and the Patient-Oriented Eczema Measure (POEM) and patient quality-of-life measurement scales.
- The POEM is a simple validated tool for measuring the severity of atopic dermatitis children and adults. POEM scores can range from 0 to 28.
- Scores of 0–2 = clear/almost clear.
- Score of 3–7 = mild atopic eczema.
- Score of 8–16 = moderate atopic eczema.
- Score of 17–24 = severe atopic eczema.
- Score of 25–28 = very severe

What are the topical treatment options available for atopic dermatitis treatment ?
- Topical corticosteroids (TCS).
- 15 g per week in an infant.
- 30 g per week in a child.
- Topical calcineurin inhibitors (TCI).
- Pimecrolimus 1% cream.
- Tacrolimus 0.03 to 0.1% ointment.
- Topical phosphodiesterase-4 (PDE-4) inhibitor
- Crisaborole.
- Wet wrap therapy( Hypothalamo-pitutary suppression may occur)
- Topical tricyclic antidepressant
- Topical doxepin.
What are the systemic treatment options available for atopic dermatitis treatment ?
- Cyclosporine
- Dupilumab.
- Methotrexate.
- Azathioprine.
- Mycophenolate mofetil.
- Systemic Corticosteroids.

How to treat atopic dermatitis (step by step approach)?
First line
- Emollients + TCS according to severity.
- After remission, shift to maintenance therapy.
- Maintenance therapy ( Emollients ± Topical TCS once weekly or TCI twice weekly).
- If no response, try the second line options.
Second line
- If no response, review triggering factors. consider diet modification in young children.
- Potent TCS may be initiated for a short period with TCI for sensitive areas.
- For severe cases, patient may need to be admitted to try wet wrap therapy or phototherapy ( not for young children).
- After remission, shift to maintenance therapy.
- If no response try the third line options
Third line
- Dupilumab
- In adults: Subcutaneous injection of 600mg initially and then 300mg every other week.
- In children ≥12 years and in adolescents:
- For patients <60 kg, start with 400 mg, followed by a maintenance dose of 200 mg every other week.
- For patients ≥60 kg, start with 600 mg, followed by a maintenance dose of 300 mg every other week.
- Short course systemic steroids
- Prednisolone (0.5 mg per kg daily).
- Tapered over several weeks to avoid flares.
- There is usually disease recurrences after cessation.
- Ciclosporin
- dose : 2.5 -3.5 mg/kg/d up to 5 mg/kg/d.
- Regular monitoring of blood pressure and renal functions are recommended.
- Azathioprine
- dose is adjusted according to TMPT activity.
- Methotrexate
- In adults; start with test dose( 5mg/week), to be increased by 2.5 mg/week up to 25 mg per week.
- In children; weekly administration of 0.3–0.5mg/kg.
- Folic acid supplementation should be given.
- Response may be noticed within 2-3 months.
- Mycophenolate mofetil
- In adults; 1-3 g/day.
- In children; 30 -50 mg/kg/day.
Does Ceramide containing emollients are beneficial for atopic dermatitis?
Ceramide containing emollients may be beneficial and helpful in repairing skin barrier but the ceramide should be provided with the addition of other 2 key physiologic lipids at an appropriate ratio, i.e., with cholesterol and ≥1 fatty acids . Otherwise it may result in barrier function deterioration *.
What is the aim of Prick skin testing in atopic patients?
- The aim is to identify specific triggers of atopic dermatitis. False results may be encountered in patients less than 8 years old.
What is the effect of use of topical steroids in children on vaccination ?
- Unless there is evidence of immunosuppression (frequent or recurrent infections or WBCs and immunoglobulin abnormalities), topical steroids have no effect on vaccines.
How to prevent atopic dermatitis in children?
- Exclusive breast feeding during the first 3-4 months of life or feeding with a formula containing exclusively hydrolyzed milk products may decrease the risk of having atopic dermatitis in babies with a family history of atopy.
- Daily use of emollients starting at the first 3 weeks of life resulted in a 30–50% reduction in the risk of having AD by 6–8 months of age in babies with a family history of atopy.
What is the role of phototherapy in treating atopic dermatitis?
- Phototherapy may improve atopic dermatitis and its associated pruritus as it induce T cell apoptosis, dendritic cells reduction and decrease Th2 cell cytokines expression.
- Narrow band UVB and UVA1 are useful for chronic lesions.
- UVA1 may help improving acute lesions.
- The patient may use phototherapy combined with topical steroids and emollients.
- Phototherapy may not be practical in young children , it is used mostly in older children and adults.
- Phototherapy course should be given once per year.
Is it risky to vaccinate atopic patients with live vaccines?
- Atopic dermatitis is not a contraindication to vaccination, but it is essential to ensure that patient is not on immunosuppressive drug.
- Short term steroid (less than 2 weeks) is not a contraindication to live vaccines administration
- Steroid of 2 mg/kg, a total of 20 mg/day prednisone may be considered immunosuppressive.
- Live vaccines may be given to patients on ( steroids more than 2 weeks, high dose steroids) at least 3 months after stoppage.
- Egg protein may be present in some vaccines but it is so small amount and it should not be a problem. If in doubt, vaccines should be given in an equipped hospital.
When to consider diet modification?
In patients with sever dermatitis who do not respond to the usual treatment and have immediate reaction to certain foods(vomiting, colic, altered bowel habits) or fail to thrive, consider food allergy.
The following food types may be incriminated in food allergy.
- Diary products.
- Beef.
- Eggs.
- Chicken.
- Fish.
- Wheat.
- citrus.
- Berry fruits.
- Food additives.
- Chocolate.
- Nuts.
In children less than 6 months of age and have severe dermatitis, exclusively hydrolyzed milk formulation may be tried and cow`s milk should be avoided.
Pediatric dietitian should be consulted.
What are the complications of atopic dermatitis?
- Infections
- Bacterial: mostly staph which may be treated with topical or systemic antibiotics and dilute bleach bathing.
- Viral :
- Herpes simplex (Eczema herpeticum).
- Molluscum contagiosum.
- Itching :
- Topical treatment .
- Topical doxepin.
- Sleep disturbance : may be treated using
- Sedating antihistamines (2nd generation antihistamines have no role in atopic dermatitis).
- Stress : refer to a psychiatrist.
- Ocular complications : refer to ophthalmologist.
Was this helpful?
20 / 0
#Atopic dermatitis #How to manage atopic dermatitis.
Thanks alot
Thanks for great informations regarding dermatological field.
You are welcome. Thank you for commenting.